
Organisations who are genuinely interested in the views and experiences of patients, families, carers and the workforce can learn from these experiences.
I was very encouraged by the new Secretary of State for health and social care Victoria Atkins MP who recently spoke about listening to patients, parents and professionals and how we need to make it easier for everyone to speak up and raise concerns throughout the system. I have been calling for ways for healthcare organisations to find it easier to listen to patients and families. I have called for all Boards to follow NICE guidance and have a patient representative, for an overhaul of the complaints process so it’s easier for patients to give feedback about their care, and more recently, for Martha’s Rule to be implemented in all acute and specialist trusts.
The circumstances around the death of Martha Mills are so shocking that we must act fast so this never happens again. Martha’s parents, Merope and Paul, were by her bedside for weeks and despite their entreaties to the healthcare professionals, their views were dismissed, ignored and they were treated disgracefully. Unfortunately since Martha died, similar examples have occurred because patients weren’t listened to and their condition deteriorated irretrievably.
Who knows their child better than the parents? How wrong it is that healthcare professionals don’t listen. There is a phrase, epistemic injustice, that describes the power differential between patients and professionals and between different professional groups so that knowledge, positional power and understanding take precedence and vital information isn’t believed or acted upon.
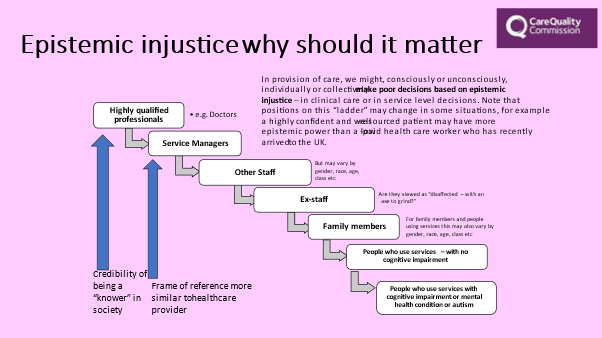
In Martha’s case, the doctors didn’t listen to the parents and other healthcare professionals who had concerns faced barriers to speaking up across a hierarchy in an environment that lacked psychological safety. The slide above shows that parents and patients, particularly those with cognitive difficulties, are the least likely to be listened to or believed.
This is what can happen when safety is considered implicitly rather than explicitly. When we know that epistemic injustice exists – and healthcare professionals who have been a patient themselves are all too aware – we need to do something about it. I’m delighted that CQC have published their guidance on human rights based inspections. And when I speak to NHS Chairs and Chief Executives they want to know what they can do, as the most senior leaders, to hear the views and voices of patients and families. They want safety to be considered explicitly and for all the systems in healthcare to be aligned improve the safety and experience of patients. There are many ways of involving and including patients as part of the clinical team, in their own care and in the design and delivery of health services.
Martha’s Rule, where patients and families can request an urgent clinical review if they feel that their concerns are not being acted upon, is at one end of the spectrum. We are working across the system to improve the way that patients can access information about their medicines and medical devices and can consent to the right treatment, knowing that their views have been listened to and taken into account.
We need a structured approach to safety, as part of a safety management system, with the ambition to be an ultrasafe industry. This relies on a leadership intent to develop a just and learning culture, where staff feel safe to speak up and flag near misses and incidents as part of business as usual. We need to move away from oppositional complaints and clinical litigation where families have to fight for the truth and there is no national system of learning from their concerns.
My vision is for a partnership approach, where the views and voices of patients and families help to prevent harm, by flagging concerns up front. And if harm occurs, a restorative approach is taken. A just and learning culture so patients receive a swift and heartfelt apology and transparency of information and patients, families, healthcare staff and the whole healthcare system are able to learn, not blame. By listening and acting on patients and families voices we can keep people safe, learn and prevent future harm.

